Table of Contents
Overview of Amoxicillin and Its Uses
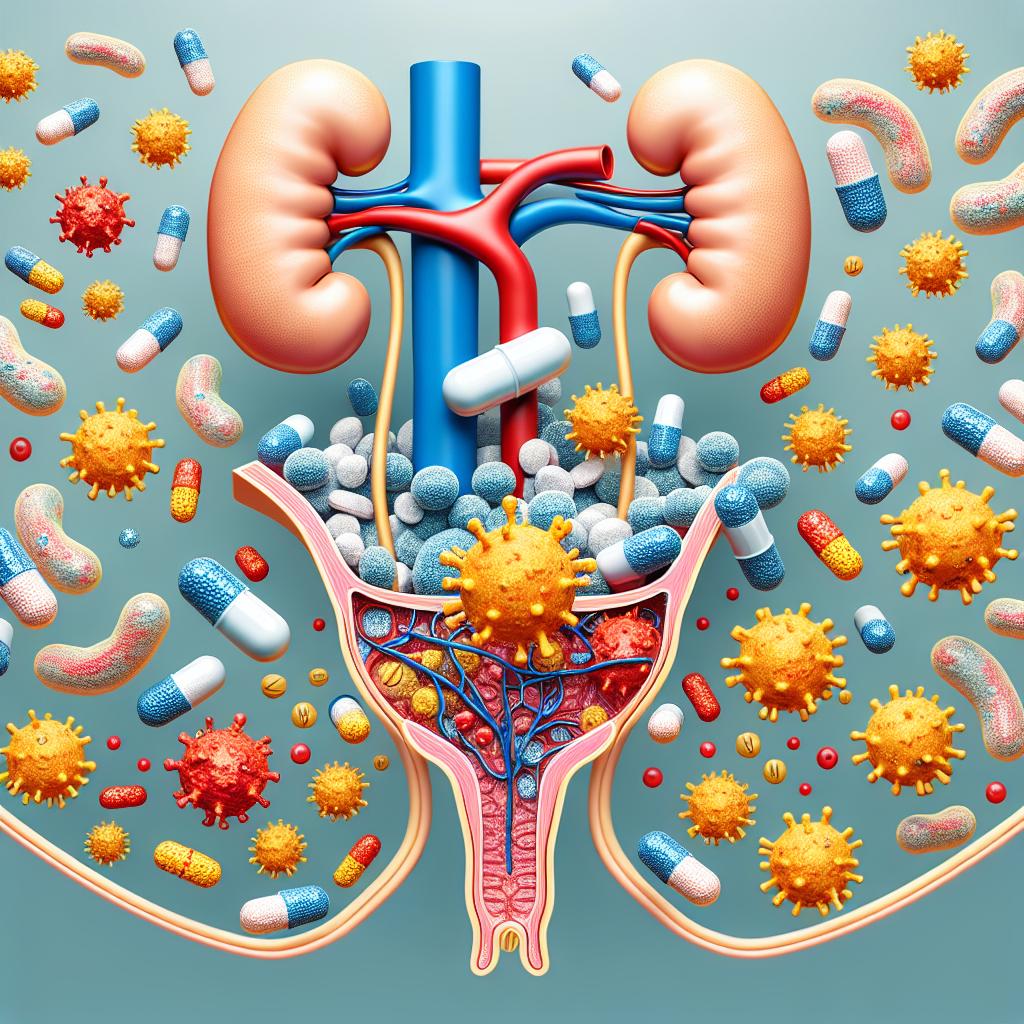
Amoxicillin is a widely prescribed antibiotic belonging to the penicillin group of drugs. It is commonly used to treat a variety of bacterial infections, including those affecting the ears, nose, throat, urinary tract, and skin. Amoxicillin works by inhibiting the growth of bacteria, effectively disrupting their cell wall synthesis, which ultimately leads to bacterial cell death. This antibiotic is particularly favored for its broad spectrum of activity, effectiveness, and favorable safety profile. According to recent studies, amoxicillin is often prescribed as a first-line treatment for uncomplicated urinary tract infections (UTIs) due to its efficacy against common uropathogens like Escherichia coli (E. coli) (Fakhri-Demeshghieh et al., 2024).
However, while amoxicillin is effective in treating bacterial infections, concerns about its usage continue to grow, particularly regarding its role in antibiotic resistance and its potential to contribute to the development of urinary tract infections (UTIs).
Potential Side Effects of Amoxicillin
Like any medication, amoxicillin comes with a range of potential side effects. Common side effects include gastrointestinal disturbances such as nausea, vomiting, and diarrhea. More serious side effects can include allergic reactions, which may manifest as rashes, itching, or anaphylaxis in rare cases. Additionally, the disruption of normal gut flora can lead to opportunistic infections, such as Clostridium difficile-associated diarrhea (C. diff), which can pose significant health risks.
One lesser-known aspect of amoxicillin use is its potential impact on the urinary tract. There is a growing body of evidence suggesting that antibiotics, including amoxicillin, can alter the normal urogenital microbiota, potentially leading to an increased risk of developing UTIs. In particular, the use of antibiotics can facilitate the overgrowth of antibiotic-resistant bacteria, which can complicate treatment and exacerbate infection rates (Ndaki et al., 2025).
Understanding Urinary Tract Infections (UTIs)
Urinary tract infections (UTIs) are among the most common bacterial infections worldwide, affecting millions of individuals each year. The condition occurs when pathogenic bacteria, often from the gastrointestinal tract, ascend into the urinary system. UTIs can be classified into uncomplicated and complicated forms. Uncomplicated Utis generally occur in healthy individuals without any underlying anatomical or functional abnormalities in the urinary tract. In contrast, complicated UTIs occur in patients with structural or functional abnormalities, such as kidney stones or urinary catheters, making them more challenging to treat (Dewachter et al., 2022).
The predominant pathogen responsible for UTIs is E. coli, accounting for approximately 80-90% of cases. Other bacteria, such as Klebsiella pneumoniae and Enterococcus faecalis, may also cause UTIs, particularly in complicated cases. Symptoms commonly associated with UTIs include frequent urination, urgency, pelvic pain, and cloudy urine. In severe cases, UTIs can lead to pyelonephritis, which is an infection of the kidneys and may require more aggressive treatment, including hospitalization (Hultgren et al., 2023).
Can Amoxicillin Trigger a UTI?
The question of whether amoxicillin can trigger a UTI is complex and multifaceted. While amoxicillin itself does not directly cause UTIs, its use can disrupt the normal flora of the urogenital tract, making it easier for pathogenic bacteria to establish infections. This disruption can lead to a condition known as dysbiosis, where the balance of bacteria in the microbiome is upset, allowing opportunistic pathogens to thrive (Shokoohizadeh et al., 2024).
Research has indicated that antibiotic use, especially broad-spectrum antibiotics like amoxicillin, can lead to an increase in antibiotic-resistant bacteria in the urinary tract. These resistant strains may be less susceptible to treatment, making UTIs more difficult to manage. A study examining the phylogroups of uropathogenic E. coli indicated that strains associated with recurrent Utis often exhibit higher antibiotic resistance profiles, including resistance to penicillins (Mahshouri et al., 2025).
Moreover, the emergence of extended-spectrum beta-lactamases (ESBLs) in E. coli and other pathogens has raised concerns regarding the treatment of UTIs. These enzymes render bacteria resistant to many beta-lactam antibiotics, including amoxicillin, complicating treatment regimens and contributing to the recurrence of infections (Kao et al., 2023).
Recommendations for Safe Amoxicillin Use
To mitigate the risks associated with amoxicillin use and its potential link to UTIs, several recommendations can be made:
-
Use Antibiotics Judiciously: Only prescribe amoxicillin when it is necessary and appropriate, based on culture and sensitivity results whenever possible.
-
Educate Patients: Inform patients about the importance of completing prescribed antibiotic courses to prevent the development of resistance and the recurrence of infections.
-
Monitor for Symptoms: Patients should be advised to monitor for symptoms of UTIs while on antibiotics, especially if they have a history of recurrent infections.
-
Consider Alternative Treatments: Explore non-antibiotic options for managing mild infections or use narrow-spectrum antibiotics when appropriate to minimize disruption of normal flora.
-
Promote Good Hygiene Practices: Encourage patients to engage in good personal hygiene practices, which can help prevent the introduction of bacteria into the urinary tract.
-
Review Antibiotic Guidelines Regularly: Healthcare providers should stay updated on local and national antibiotic prescribing guidelines, adjusting their practices based on local resistance patterns.
-
Conduct Regular Surveillance: Facilities should conduct regular surveillance of antibiotic resistance patterns to inform empirical therapy and help reduce the incidence of resistant infections.
FAQs
Can amoxicillin cause a UTI?
Amoxicillin itself does not directly cause a UTI, but its use can disrupt the normal urinary microbiota, increasing the risk of bacterial overgrowth and infection.
What are the common side effects of amoxicillin?
Common side effects include gastrointestinal issues like nausea, vomiting, diarrhea, and potential allergic reactions. Disruption of gut flora can also lead to opportunistic infections.
How can I prevent UTIs while using amoxicillin?
To prevent UTIs, practice good hygiene, stay hydrated, and follow your healthcare provider’s advice regarding antibiotic use.
What should I do if I develop symptoms of a UTI while on amoxicillin?
If you experience symptoms of a UTI, contact your healthcare provider for further evaluation and possible adjustment of your treatment plan.
References
- Fakhri-Demeshghieh, A., Shokri, A., Bokaie, S., & et al. (2024). Antibiotic resistance of Uropathogenic Escherichia coli (UPEC) among Iranian pediatrics: systematic review and Meta-analysis. Iranian Journal of Public Health, 53(3), 508-523. https://doi.org/10.30699/ijmm.16.1.56
- Ndaki, P. M., Mwanga, J. R., Mushi, M. F., & et al. (2025). Drivers of inappropriate use of antibiotics among community members in low- and middle-income countries: a systematic review of qualitative studies. BMC Public Health, 25(1), 21553. https://doi.org/10.1186/s12889-025-21553-6
- Hultgren, S. J., et al. (2023). Uropathogenic Escherichia coli: Evolutionary Strategies in Urine. Nature Reviews Microbiology, 21(7), 450-466
- Mahshouri, P., Alikhani, M. Y., & et al. (2025). Analysis of phylogroups, biofilm formation, virulence factors, antibiotic resistance and molecular typing of uropathogenic Escherichia coli strains isolated from patients with recurrent and non-recurrent urinary tract infections. BMC Infectious Diseases, 25(1), 10635. https://doi.org/10.1186/s12879-025-10635-w
- Kao, C. Y., Zhang, Y. Z., Yang, D. C., & et al. (2023). Characterization of host and Escherichia coli strains causing recurrent urinary tract infections based on molecular typing. BMC Microbiology, 23(1), 190. https://doi.org/10.1186/s12866-023-02820-1