Table of Contents
Symptoms of Yeast Infections: What to Watch For
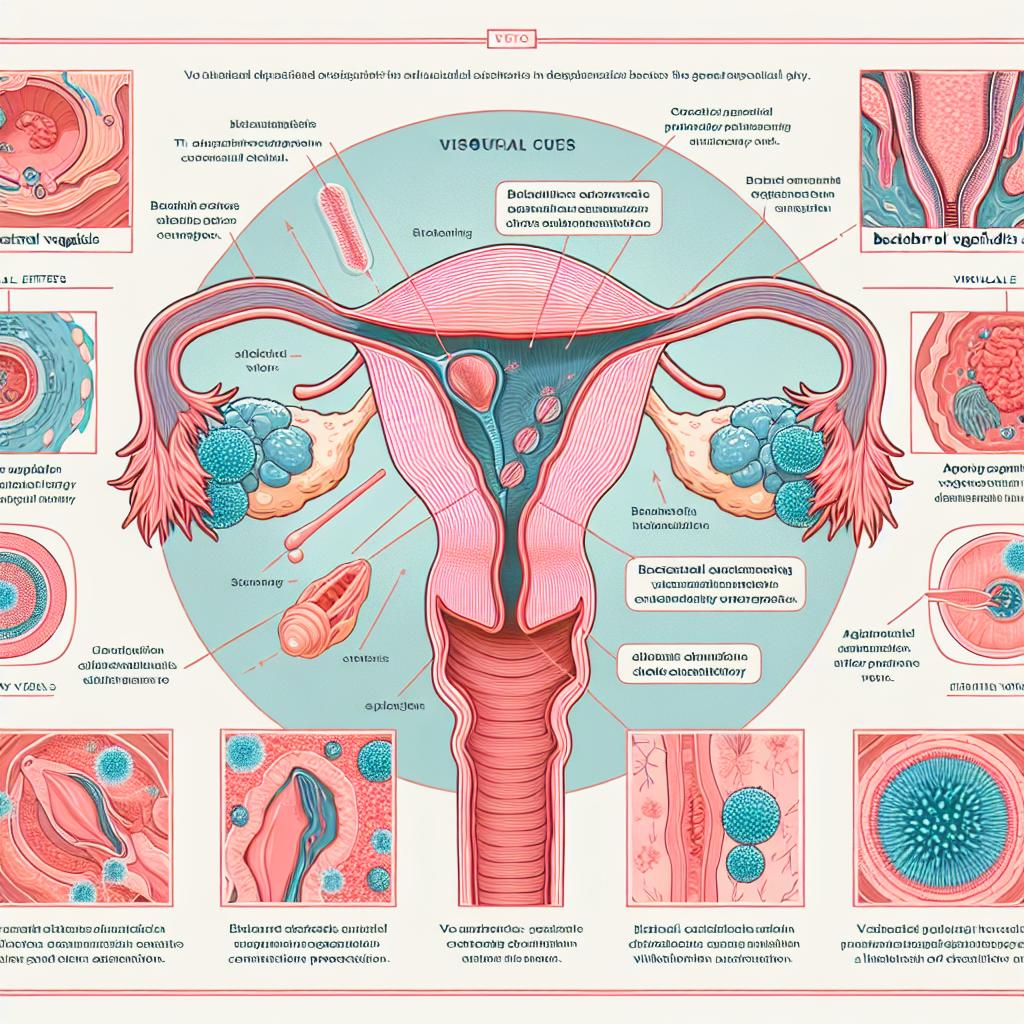
Yeast infections manifest through several symptoms that can vary in intensity and type. The most typical symptoms include:
-
Itching and Irritation: The most common symptom is a persistent itching sensation in the affected area, which can be quite uncomfortable. This itching is usually accompanied by irritation and redness of the skin.
-
Unusual Discharge: Yeast infections often cause a thick, white discharge that resembles cottage cheese. This discharge is typically odorless, which distinguishes it from other types of infections that may have a foul smell.
-
Pain During Intercourse: Many women report experiencing pain during sexual intercourse, which can be a significant concern and lead to decreased sexual activity.
-
Burning Sensation: A burning sensation during urination is another symptom that can occur, making it uncomfortable to urinate.
-
Swelling and Redness: The vulva and surrounding areas may appear swollen and red, indicating inflammation caused by the infection.
Recognizing these symptoms early is essential for effective treatment. If you experience these signs, it is advisable to consult a healthcare professional for an accurate diagnosis and appropriate intervention.
How Yeast Infections Can Affect Your Health
While yeast infections are typically not life-threatening, they can impact your overall health and well-being. Chronic or recurrent yeast infections can lead to:
-
Emotional Distress: Persistent symptoms can cause emotional and psychological distress, leading to anxiety and decreased quality of life.
-
Compromised Sexual Health: The discomfort associated with yeast infections can affect sexual relationships, leading to avoidance of sexual activity due to pain or embarrassment.
-
Increased Risk of Other Infections: Yeast infections can sometimes signal an underlying health issue, such as diabetes or a weakened immune system. This can lead to an increased risk of other infections.
-
Antibiotic Resistance: Overuse of antifungal medications can lead to resistance, making treatment more complicated for future infections.
Understanding these implications highlights the importance of seeking treatment and managing yeast infections effectively.
The Connection Between Yeast Infections and Bleeding
One of the more concerning symptoms that some individuals may experience is bleeding. While bleeding is not a typical symptom of a yeast infection, it can occur under certain circumstances. Here are some potential connections:
-
Inflammation and Irritation: The intense itching and irritation caused by a yeast infection can lead to scratching or inflammation, which may result in minor bleeding.
-
Coinciding Conditions: Sometimes, individuals may experience a yeast infection alongside other conditions, such as bacterial vaginosis or sexually transmitted infections (STIs), which could lead to bleeding. These coexisting conditions can cause inflammation and irritation that may result in bleeding.
-
Hormonal Changes: Hormonal fluctuations, particularly during menstruation, can also exacerbate symptoms of a yeast infection. Some women may notice bleeding that coincides with their menstrual cycle, which could be misattributed to the infection.
-
Severity of Infection: In rare cases, severe yeast infections can lead to more pronounced inflammation, potentially causing bleeding.
If you experience any bleeding along with symptoms of a yeast infection, it is essential to consult a healthcare professional to rule out other potential causes and ensure appropriate treatment.
When to Seek Medical Attention for Yeast Infection Symptoms
While many yeast infections can be treated effectively with over-the-counter antifungal medications, there are circumstances under which you should seek medical attention. It’s crucial to be aware of these signs:
-
Persistent Symptoms: If symptoms persist for more than a few days despite treatment, it may indicate a more severe or resistant infection.
-
Severe Pain or Discomfort: If you experience severe pain, especially during urination or sexual intercourse, it is vital to seek medical help.
-
Bleeding: Any unexplained bleeding accompanying yeast infection symptoms should be evaluated by a healthcare provider. This is particularly important if the bleeding is heavy or occurs outside of your menstrual cycle.
-
Recurrent Infections: If you find yourself experiencing recurrent yeast infections (four or more in a year), it is essential to seek medical advice to identify any underlying health issues that may be contributing to the problem.
-
Underlying Health Conditions: Individuals with diabetes, compromised immune systems, or other chronic health conditions should consult a healthcare professional if they suspect a yeast infection.
By recognizing these warning signs, you can take proactive steps to protect your health and well-being.
Treatment Options for Yeast Infections and Associated Symptoms
Treating yeast infections effectively involves various options, from over-the-counter medications to prescription treatments. Here’s a detailed overview of the available treatments:
-
Over-the-Counter Antifungal Medications: Many yeast infections can be treated with topical or oral antifungal medications available without a prescription. Common active ingredients include clotrimazole, miconazole, and fluconazole. These medications are effective for most uncomplicated yeast infections.
-
Prescription Antifungal Medications: In cases of severe or recurrent infections, a healthcare provider may prescribe stronger antifungal medications such as ketoconazole or terconazole. These medications may be necessary to eliminate the infection effectively.
-
Home Remedies: Some individuals seek natural remedies for yeast infections. While certain home treatments, such as probiotics or yogurt, may help restore vaginal flora, they should not replace medical advice. Always consult a healthcare professional before trying these methods.
-
Lifestyle Modifications: Making dietary changes, such as reducing sugar intake, may help prevent future infections. Additionally, wearing breathable cotton underwear and avoiding irritants like scented products can promote vaginal health.
-
Addressing Underlying Conditions: For those with recurrent yeast infections, it is crucial to identify and treat any underlying health issues, such as uncontrolled diabetes or hormonal imbalances.
In addition to these treatment options, it is essential to adopt preventive measures to reduce the risk of future infections. Practicing good hygiene, maintaining a balanced diet, and avoiding unnecessary antibiotic use can all contribute to better vaginal health.
FAQ Section
Can a yeast infection cause heavy bleeding?
While a yeast infection typically does not cause heavy bleeding, minor bleeding can occur due to irritation or inflammation. If you experience heavy bleeding, consult a healthcare provider to rule out other conditions.
How long does a yeast infection last?
Most yeast infections can be effectively treated within a few days to a week with appropriate antifungal medications. However, persistent symptoms may require further medical evaluation.
Are yeast infections contagious?
Yeast infections are not considered sexually transmitted and are not contagious. However, the yeast can be passed between partners, so it is advisable to avoid sexual activity until the infection is treated.
Can stress cause yeast infections?
Stress can weaken the immune system, potentially increasing the risk of developing a yeast infection. Managing stress through healthy coping mechanisms may help reduce the likelihood of infections.
When should I see a doctor for a yeast infection?
You should see a doctor if you experience persistent symptoms, severe pain, unexplained bleeding, or recurrent infections. A healthcare professional can help determine the cause and appropriate treatment.
References
- Centers for Disease Control and Prevention. (2023). Vaginal Yeast Infections
- National Institutes of Health. (2022). Yeast Infections: Symptoms and Treatment
- American College of Obstetricians and Gynecologists. (2023). Vaginal Infections and STIs: What You Need to Know
- Mayo Clinic. (2023). Yeast Infection
- World Health Organization. (2023). Fungal Infections