Table of Contents
Symptoms of Bacterial Vaginosis
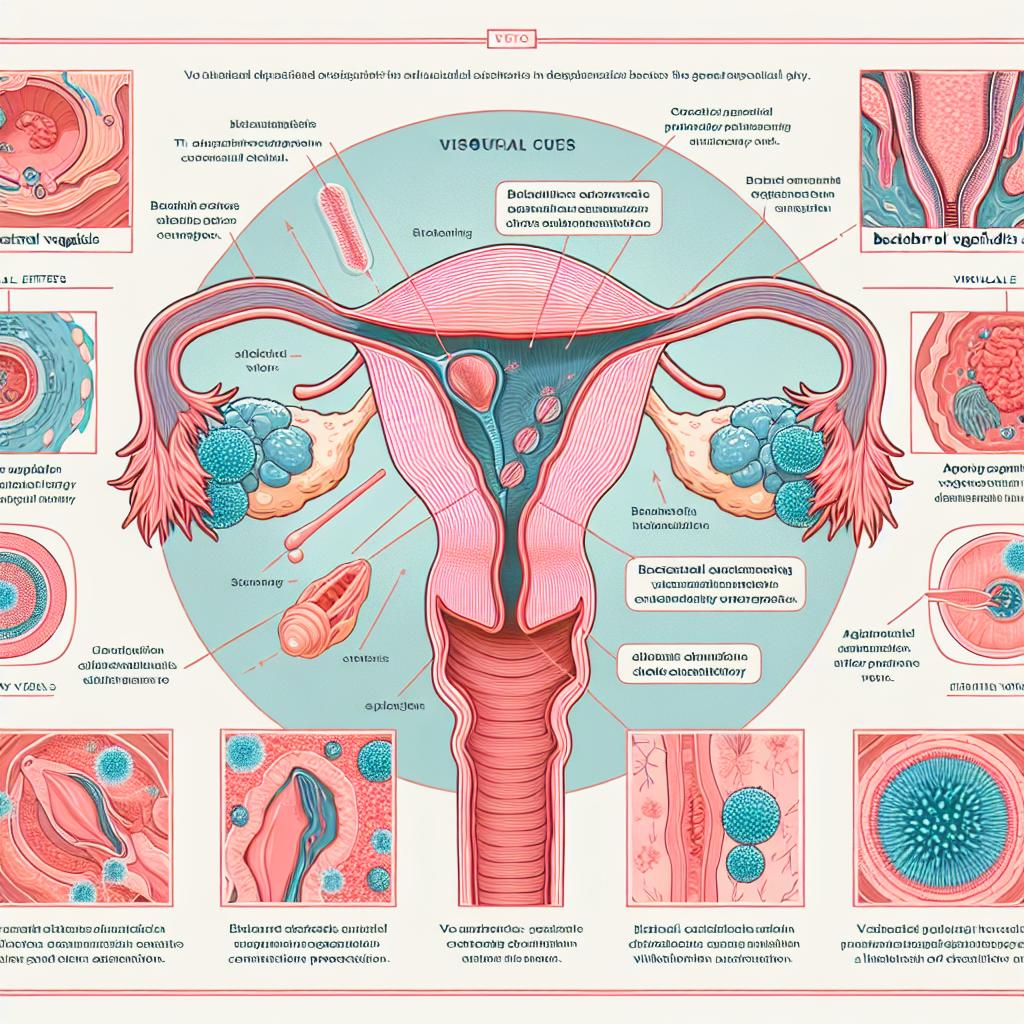
Bacterial vaginosis is characterized by an imbalance in the normal bacterial flora of the vagina, primarily a decrease in Lactobacilli and an increase in anaerobic bacteria such as Gardnerella vaginalis. Common symptoms include:
- Vaginal Discharge: A thin, grayish-white discharge is often noted, which may have a fishy odor, especially after sexual intercourse.
- Itching and Irritation: Some women may experience mild itching or irritation in the vaginal area, although many cases are asymptomatic.
- Vaginal pH Changes: The pH level in cases of BV is typically greater than 4.5, as opposed to the normal acidic range of 3.8 to 4.5 due to Lactobacilli activity.
Symptoms of Trichomoniasis
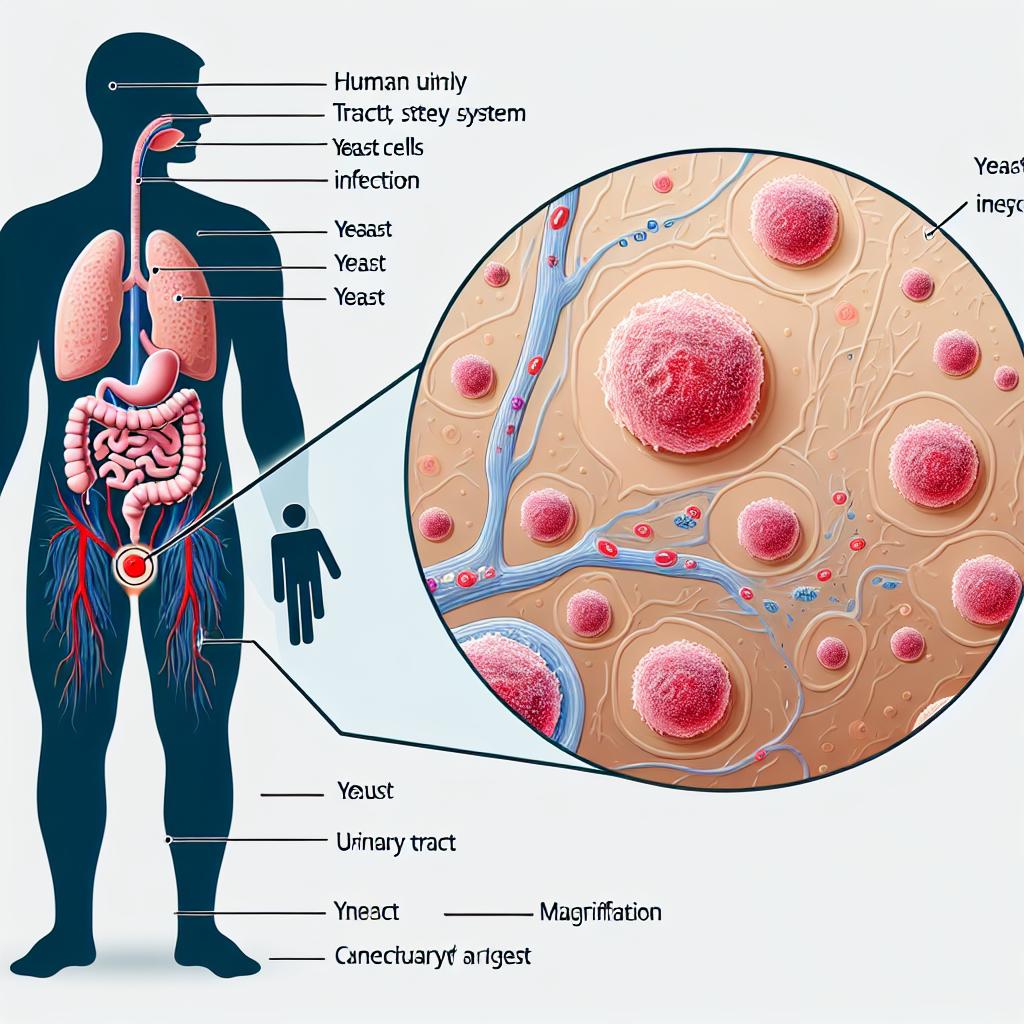
Trichomoniasis is caused by the protozoan parasite Trichomonas vaginalis. The symptoms can be more pronounced and include:
- Discharge: A frothy, yellow-green discharge with a strong odor is a hallmark of Trich infection.
- Itching and Discomfort: Patients often report significant vaginal itching, irritation, and even pain during intercourse or urination.
- Strawberry Appearance: During a gynecological examination, the cervix may exhibit a “strawberry” appearance, indicative of inflammation.
Diagnosis
Diagnosis of BV typically involves a pelvic exam, where a clinician may observe the characteristic discharge and conduct tests such as the Amsel criteria or Nugent scoring. In contrast, Trichomoniasis can be diagnosed through a wet mount examination, where the parasite can often be observed under a microscope, or through nucleic acid amplification tests (NAAT) for higher accuracy.
Table 1: Comparison of BV and Trich Symptoms and Diagnosis
| Symptom/Characteristic | Bacterial Vaginosis | Trichomoniasis |
|---|---|---|
| Vaginal Discharge | Thin, grayish-white, fishy odor | Frothy, yellow-green, strong odor |
| Itching | Mild, if present | Significant, often severe |
| Pain during Urination | Rarely reported | Commonly reported |
| Cervical Appearance | Normal | “Strawberry” appearance |
| Diagnosis | Amsel criteria, Nugent scoring | Wet mount, NAAT |
Treatment Options for BV and Trich: What You Need to Know
Both BV and Trichomoniasis require specific treatment regimens to mitigate symptoms and prevent complications. Understanding these options can aid in timely intervention.
Treatment for Bacterial Vaginosis
The most common treatments for BV include:
-
Antibiotics: Metronidazole and clindamycin are the primary antibiotics used, prescribed either orally or topically.
- Efficacy: Studies show that approximately 70-80% of women respond to treatment, although recurrence is common within three months post-treatment (Klebanoff et al., 2023; reference 6).
-
Probiotics: Emerging research suggests that probiotics may help restore healthy vaginal flora, though more extensive studies are needed to establish efficacy.
Treatment for Trichomoniasis
Trichomoniasis is typically treated with:
-
Antimicrobial Medications: Metronidazole or tinidazole are the first-line treatments, usually administered as a single dose.
- Efficacy: These treatments are highly effective, with cure rates exceeding 95% after a single dose in most cases (Schumann et al., 2024; reference 7).
-
Partner Treatment: It is crucial for sexual partners to be treated simultaneously to prevent reinfection.
Table 2: Treatment Comparison for BV and Trich
| Condition | Treatment Options | Administration | Cure Rate |
|---|---|---|---|
| Bacterial Vaginosis | Metronidazole, Clindamycin | Oral or topical | 70-80% |
| Trichomoniasis | Metronidazole, Tinidazole | Single dose oral | >95% |
Prevention Strategies for BV and Trich: Effective Practices
Preventing BV and Trich involves understanding risk factors and implementing effective strategies.
Prevention of Bacterial Vaginosis
- Avoid Douching: This practice disrupts normal flora and increases the risk of BV.
- Use Protection: Safe sex practices, including condom use, can reduce the risk of both BV and other STIs.
- Maintain Hygiene: Regular bathing and wearing breathable cotton underwear can help maintain a healthy vaginal environment.
Prevention of Trichomoniasis
- Regular STI Screening: Women with multiple sexual partners should consider regular screening for STIs, including Trich.
- Partner Communication: Discussing STI testing and sexual health with partners can help mitigate risks.
- Limit Sexual Partners: Reducing the number of sexual partners can decrease the likelihood of infection.
Table 3: Preventive Measures for BV and Trich
| Infection | Preventive Measures |
|---|---|
| Bacterial Vaginosis | Avoid douching, use protection, maintain hygiene |
| Trichomoniasis | Regular STI screening, partner communication, limit sexual partners |
The Impact of BV and Trich on Pregnancy Outcomes
Pregnancy outcomes can be significantly impacted by infections such as BV and Trich. Understanding these risks is crucial for expecting mothers.
Bacterial Vaginosis and Pregnancy
- Preterm Birth: Studies indicate that BV is associated with a higher risk of preterm birth and low birth weight (Yao et al., 2025; reference 8).
- Intrauterine Infections: The presence of BV can lead to ascending infections that may compromise fetal health.
Trichomoniasis and Pregnancy
- Increased Risks: Pregnant women with Trich are at an elevated risk for preterm labor, low birth weight, and premature rupture of membranes (Yao et al., 2025; reference 8).
- Maternal Health Complications: Trich can lead to complications that may affect maternal health and overall pregnancy outcomes.
Table 4: Pregnancy Risks Associated with BV and Trich
| Infection | Risks |
|---|---|
| Bacterial Vaginosis | Preterm birth, low birth weight, intrauterine infections |
| Trichomoniasis | Preterm labor, low birth weight, premature rupture of membranes |
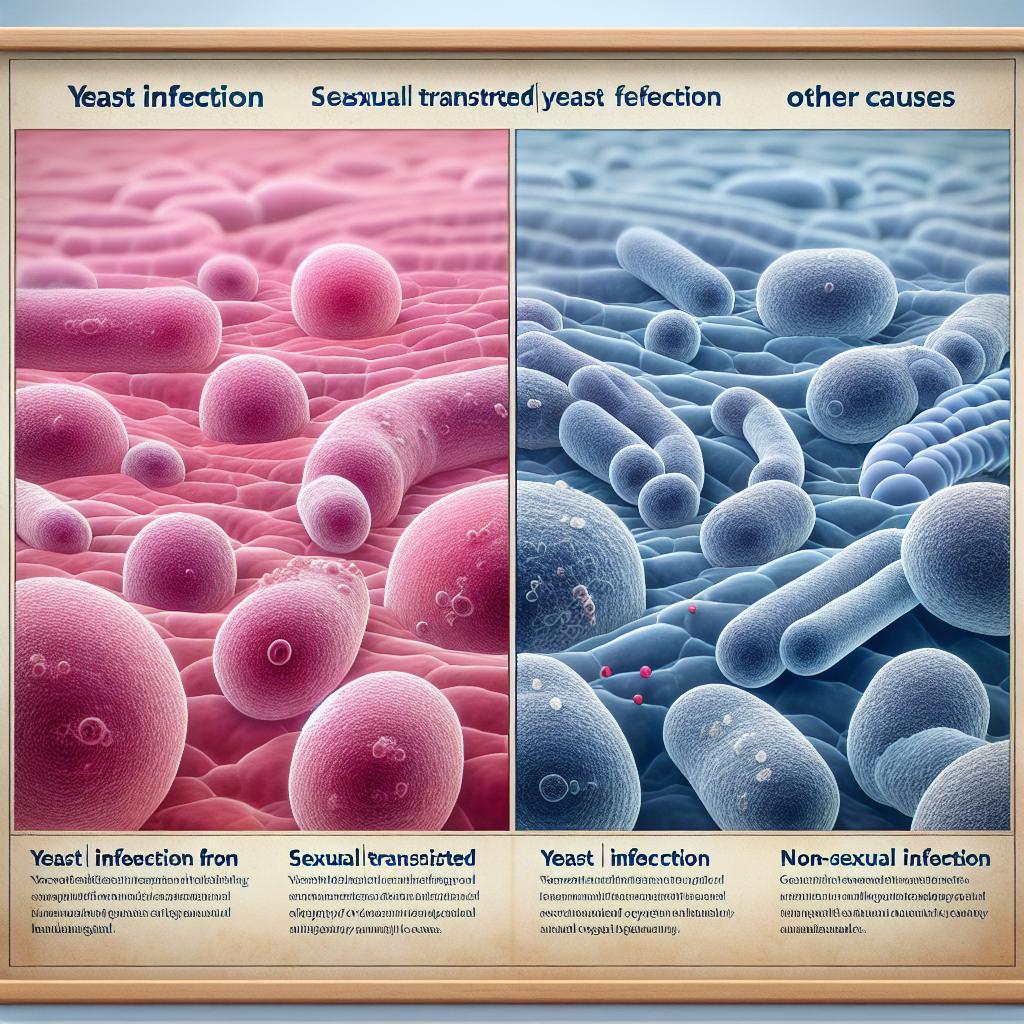
Understanding the Relationship Between BV, Trich, and STIs
The interplay between BV, Trich, and other sexually transmitted infections (STIs) is complex and significant.
Co-Infections
Women with BV are at a higher risk of acquiring STIs, including Trichomoniasis. Conversely, infections like Trich can exacerbate the symptoms of BV, leading to a cycle of recurrent infections.
Implications for Treatment
- Dual Therapy: Given the potential for co-infection, healthcare providers may recommend combination therapy for women diagnosed with both conditions to ensure comprehensive treatment and management.
- Screening Recommendations: Regular screening for STIs is essential, particularly for women diagnosed with BV, to mitigate risks and promote reproductive health.
Table 5: Relationships Between BV, Trich, and STIs
| Condition | Associated Risks |
|---|---|
| Bacterial Vaginosis | Increased risk of STIs, including Trich |
| Trichomoniasis | Exacerbation of BV symptoms, higher risk of STIs |
FAQ
What is the main cause of bacterial vaginosis?
Bacterial vaginosis is primarily caused by an imbalance in the normal bacterial flora of the vagina, where harmful bacteria outnumber beneficial Lactobacilli.
How is trichomoniasis transmitted?
Trichomoniasis is transmitted through sexual contact, including vaginal, oral, or anal sex with an infected partner.
Can bacterial vaginosis affect pregnancy?
Yes, bacterial vaginosis can increase the risk of preterm birth, low birth weight, and other complications during pregnancy.
How is bacterial vaginosis diagnosed?
Bacterial vaginosis is diagnosed through a pelvic examination, assessment of vaginal discharge, and laboratory tests such as the Amsel criteria or Nugent scoring.
What are the treatment options for trichomoniasis?
Trichomoniasis is typically treated with antibiotics such as metronidazole or tinidazole, often administered as a single dose.
References
-
Klebanoff, M. A., Schuit, E., Lamont, R. F., Larsson, P. G., Odendaal, H. J., Ugwumadu, A., Kiss, H., Petricevic, L., Andrews, W. W., & Hoffman, M. K. (2023). Antibiotic treatment of bacterial vaginosis to prevent preterm delivery: Systematic review and individual participant data meta-analysis. Paediatr Perinat Epidemiol, 37(3), 239–251. doi:10.1111/ppe.12947
-
Schumann, J. A., & Plasner, S. (2024). Trichomoniasis. StatPearls
-
Yao, D., Dongting, T., Xinyu, Z., Minghui, X., Keyu, Z., Wei, L., Ze, C., Meng, N., Baihe, L., Yanan, T., Zhenying, L., Chunyu, C., Yi, H., Xiaorui, L., Qianqian, Z., Jiuru, Z., & Haiou, Y. (2025). The effects of vaginal infections on pregnancy outcomes: a retrospective cohort study in China. BMC Pregnancy Childbirth, 25, 73–109. doi:10.1186/s12884-025-07309-5
-
Sorano, S., Chaponda, E., Banda, E., Mirandola, M., Chikwanda, E., Mwewa, V., Mulenga, J. M., & Unemo, M. (2025). Diagnostic accuracy of an antigen-based point-of-care test versus nucleic acid amplification testing for genital trichomoniasis among pregnant women attending antenatal care facilities in Zambia. BMC Infect Dis, 25, 10698–10698. doi:10.1186/s12879-025-10698-9
-
Eslami, M., Naderian, R., Ahmadpour, A., Shushtari, A., Maleki, S., Mohammadian, P., Amiri, A., Janbazi, M., Memarian, M., & Yousefi, B. (2024). Microbiome structure in healthy and pregnant women and importance of vaginal dysbiosis in spontaneous abortion. Front Cell Infect Microbiol, 14, 1401610. doi:10.3389/fcimb.2024.1401610
-
Elnashar, A. (2021). Impact of endometrial microbiome on fertility. Middle East Fertility Soc J, 26(4), 4. doi:10.1186/s43043-020-00050-3
-
Donders, G. (2011). Aerobic vaginitis in pregnancy. BJOG, 118(10), 1163–1170. doi:10.1111/j.1471-0528.2011.03020.x
-
Kenfack-Zanguim, J., Kenmoe, S., Bowo-Ngandji, A., Kenfack-Momo, R., Thierry Ebogo-Belobo, J., Kengne-Ndé, C., Serge Mbaga, D., Zeuko’o Menkem, E., Lontuo Fogang, R., & Tchatchouang, S. (2023). Systematic review and meta-analysis of maternal and fetal outcomes among pregnant women with bacterial vaginosis. Eur J Obstet Gynecol Reprod Biol, 289, 9–18. doi:10.1016/j.ejogrb.2023.08.013
-
Gigi, R. M. S., Buitrago-Garcia, D., Taghavi, K., Dunaiski, C. M., van de Wijgert, J. H. H. M., Peters, R. P. H., & Low, N. (2023). Vulvovaginal yeast infections during pregnancy and perinatal outcomes: systematic review and meta-analysis. BMC Womens Health, 23(1), 116. doi:10.1186/s12905-023-02258-7
-
Abele-Horn, M., Scholz, M., Wolff, C., Kolben, M. (2000). High-density vaginal Ureaplasma urealyticum colonization as a risk factor for chorioamnionitis and preterm delivery. Acta Obstet Gynecol Scand, 79(11), 973–978. doi:10.1007/s00404-017-4331-y
-
Dai, T., Zhang, Z., & Chen, Y. (2021). Dysbiosis of gut microbiota is associated with renal carcinoma. Front Cell Infect Microbiol, 11, 609488. doi:10.3389/fcimb.2021.609488
-
Banerjee, S., & Ranjan, K. (2022). The role of microbiota in the pathogenesis of ovarian cancer. Int J Mol Sci, 23(3), 1163. doi:10.3390/ijms23031163