Table of Contents
What is a Bladder Infection?
A bladder infection, medically termed cystitis, is a form of urinary tract infection (UTI) that specifically affects the bladder. It occurs when bacteria enter the urinary system, multiply, and cause inflammation. Bladder infections are among the most common types of UTIs and can result in various uncomfortable symptoms. The condition predominantly affects women, although men can also get bladder infections.
Symptoms of a bladder infection include frequent urination, a strong urge to urinate, a burning sensation during urination, and cloudy or strong-smelling urine. In some cases, there might be blood in the urine (hematuria) or pelvic pain. If left untreated, a bladder infection can lead to more serious complications, including a kidney infection, which is significantly more severe.
Understanding Urinary Tract Infections (UTIs)
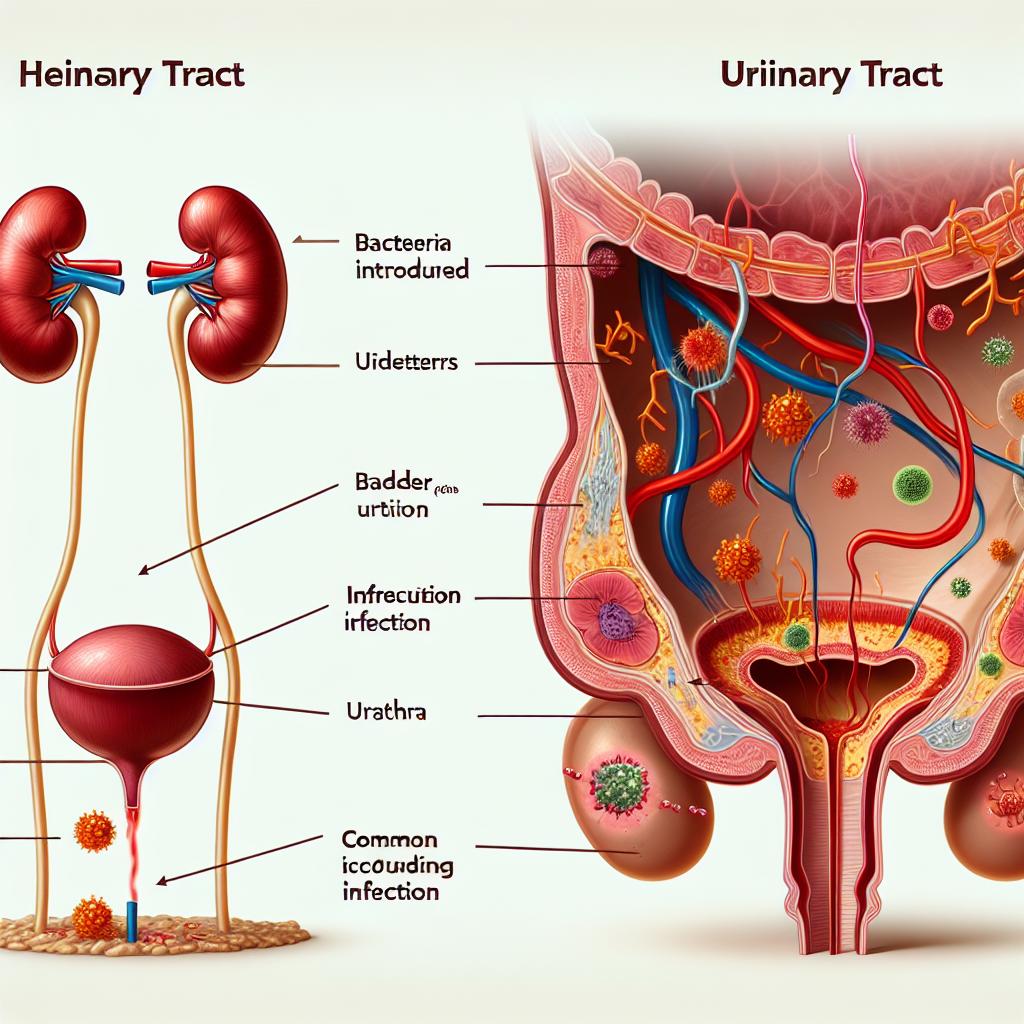
Urinary tract infections encompass infections that can occur in any part of the urinary system, which includes the kidneys, ureters, bladder, and urethra. UTIs are classified into two main categories: upper UTIs, which involve the kidneys (pyelonephritis), and lower UTIs, which primarily affect the bladder and urethra.
The most common causative agent of UTIs is Escherichia coli (E. coli), a bacterium that is naturally found in the intestines. However, other bacteria can also cause UTIs, particularly in patients with specific risk factors such as diabetes, urinary tract abnormalities, or those who have undergone recent urinary procedures.
Individuals may experience a range of symptoms, from mild discomfort to severe pain. Common symptoms include:
- Frequent and urgent need to urinate
- Pain or burning sensation during urination
- Cloudy or foul-smelling urine
- Lower abdominal pain or pressure
- Fever and chills (in cases of kidney infections)
Symptoms: Bladder Infection vs UTI
While bladder infections and UTIs share many symptoms, there are key differences worth noting. Bladder infections typically present with localized symptoms related to bladder irritation, whereas UTIs involving the upper urinary tract may present more systemic symptoms.
| Symptom | Bladder Infection | Upper UTI (Kidney Infection) |
|---|---|---|
| Frequent urination | Yes | Yes |
| Urgency to urinate | Yes | Yes |
| Burning sensation during urination | Yes | Yes |
| Lower abdominal pain | Yes | Yes |
| Flank pain | No | Yes |
| Fever | Rarely | Yes |
| Nausea or vomiting | No | Yes |
| Blood in urine | Yes | Yes |
Understanding these differences is crucial for appropriate diagnosis and treatment.
Causes and Risk Factors for Bladder Infections and UTIs
Bladder infections and UTIs can arise from various factors, including:
- Bacterial Introduction: Most UTIs occur when bacteria enter the urinary tract, often through the urethra.
- Sexual Activity: Increased sexual activity can promote the introduction of bacteria into the urinary tract.
- Urinary Catheters: Catheterization can introduce bacteria directly into the bladder.
- Hormonal Changes: Changes, especially in women during menopause, can alter the vaginal flora and increase the risk of infection.
- Diabetes: Individuals with diabetes are more susceptible to infections due to compromised immune responses.
- Urinary Tract Abnormalities: Structural abnormalities can impede normal urine flow, leading to increased risk of infection.
- Inadequate Fluid Intake: Low fluid intake can result in concentrated urine, which can irritate the bladder and promote bacterial growth.
Treatment Options for Bladder Infections and UTIs
Treatment for bladder infections and UTIs typically involves antibiotics to eliminate the underlying infection. The choice of antibiotic depends on the specific bacteria identified and its resistance profile. Commonly prescribed antibiotics include:
- Trimethoprim-sulfamethoxazole: Often used for uncomplicated UTIs.
- Nitrofurantoin: Particularly effective for bladder infections.
- Fosfomycin: Useful for single-dose treatment.
- Fluoroquinolones: Effective but may be reserved for more complicated cases due to potential side effects.
In addition to antibiotics, patients are often advised to increase fluid intake to help flush out the bacteria and reduce symptoms. Pain relievers such as phenazopyridine can also be used to alleviate burning and discomfort.
For recurrent infections, further evaluation may be warranted, including imaging studies or urological examination, to identify any underlying anatomical issues.
Conclusion
Understanding the differences between bladder infections and urinary tract infections is crucial for effective management and treatment. Both conditions can significantly impact quality of life, but with timely diagnosis and appropriate treatment, patients can experience relief and reduce the risk of complications.
FAQ
Can a bladder infection lead to a UTI?
Yes, a bladder infection is a type of UTI. All bladder infections are UTIs, but not all UTIs are bladder infections.
How can I prevent bladder infections?
Preventive measures include drinking plenty of fluids, urinating after sexual intercourse, avoiding irritating feminine products, and maintaining good hygiene.
Are bladder infections serious?
While bladder infections are common and often easily treated, they can lead to more severe complications if left untreated, such as kidney infections.
How long does it take for antibiotics to work for a bladder infection?
Many patients start to feel better within a few days of starting antibiotics, but it’s crucial to complete the full course as prescribed.
References
-
Amundsen, C. L., Sutherland, S. E., Kielb, S. J., & Dmochowski, R. R. (2024). Sacral and Implantable Tibial Neuromodulation for the Management of Overactive Bladder: A Systematic Review and Meta-analysis. https://doi.org/10.1007/s12325-024-03019-0
-
Al-Azzawi, I. S., & Al-Hindawi, H. T. (2020). A comparative study between sacral neuromodulation and intravesical botulinum toxin injection for patients with refractory overactive bladder. Arab J Urol. https://pubmed.ncbi.nlm.nih.gov/11771483/
-
Dreyfuss, L. D., Nik-Ahd, F., Wang, L., Shatkin-Margolis, A., Covinsky, K., & John Boscardin, W. (2024). Sacral neuromodulation in nursing home residents: predictors of success and complications in a national cohort of older adults. Neurourol Urodyn. https://pubmed.ncbi.nlm.nih.gov/11771491/
-
Doersch, K. M., Gonzalez, R., Flynn, B. J., & Kukreja, J. B. (2025). Improving safety in the performance of robotic urinary diversions: a narrative review. https://pubmed.ncbi.nlm.nih.gov/11770738/
-
Lashin, A. M., Eltabey, N. A., & Wadie, B. S. (2024). Case Report: Management of a case of multidrug-resistant Klebsiella pneumoniae infection in a second-kidney transplant patient. https://doi.org/10.3389/frtra.2024.1494016
-
Cacciamani, G. E., & D’Hondt, F. (2023). The usage of the Paris classification system in urine cytology in the diagnosis of non-muscle-invasive bladder cancer: a retrospective single-center study. https://doi.org/10.1007/s12672-025-01828-5