Table of Contents
Overview of Urogenital Flora and Infections
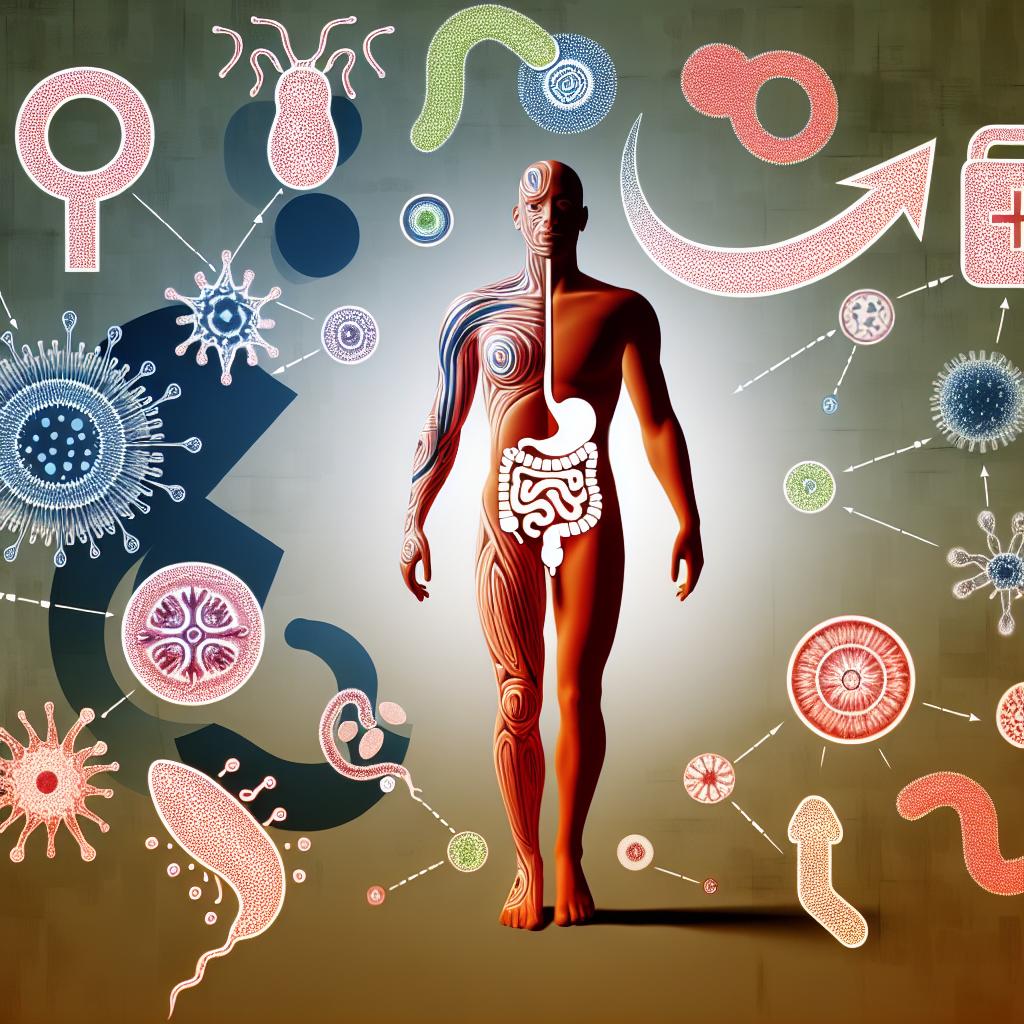
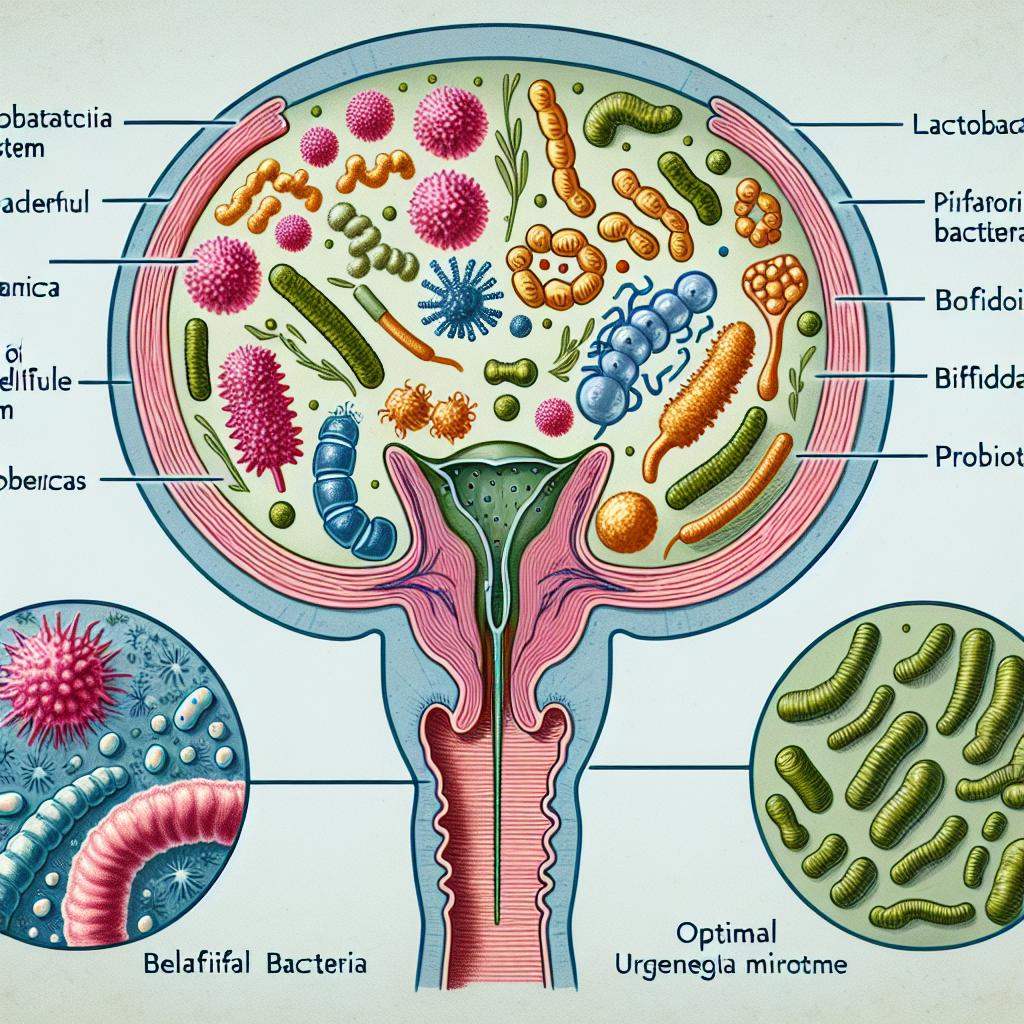
The urogenital tract hosts a complex and diverse microbiome, which plays a crucial role in maintaining the health of the reproductive and urinary systems. This ecosystem is primarily dominated by various bacterial species, including Lactobacillus, Gardnerella, and Ureaplasma. However, disturbances in this delicate balance can lead to infections, commonly caused by sexually transmitted pathogens such as Chlamydia trachomatis, Neisseria gonorrhoeae, and Mycoplasma genitalium (Werner et al., 2025).
Infections in the urogenital tract can present with a range of clinical symptoms, including dysuria, urethral discharge, and pelvic pain. The lack of specific symptoms often complicates timely diagnosis and treatment, resulting in significant public health concerns due to potential complications such as infertility and chronic pelvic pain (Rodrigues et al., 2025). The microbiological diversity within the urogenital flora indicates that mixed infections are prevalent. Therefore, understanding the implications of antibiotic treatment for these mixed urogenital flora infections is vital for effective management.
Common Pathogens in Mixed Urogenital Infections
Mixed urogenital infections often involve multiple pathogens, making treatment challenging. The presence of Chlamydia trachomatis is particularly concerning as it is one of the most common sexually transmitted infections (STIs) worldwide, with an increasing incidence reported in various regions (Rodrigues et al., 2025). In a recent study, it was found that Chlamydia trachomatis infections are associated with significant reproductive health risks, including pelvic inflammatory disease and infertility (Rodrigues et al., 2025).
Other common pathogens that are frequently detected alongside Chlamydia trachomatis include:
- Neisseria gonorrhoeae: Known for causing gonorrhea, this bacterium can lead to severe complications if left untreated.
- Mycoplasma genitalium: An emerging pathogen that has been linked to non-gonococcal urethritis and is associated with increased rates of infertility (Rodrigues et al., 2025).
- Ureaplasma urealyticum: Often detected in conjunction with other pathogens, this microbe is a common inhabitant of the urogenital tract.
These pathogens can create a complex infection environment, necessitating a nuanced approach to treatment that considers the potential for antibiotic resistance and the need for broad-spectrum coverage.
Importance of Targeted Antibiotic Therapy
Targeted antibiotic therapy is essential for effectively managing mixed urogenital infections. Empirical treatment often begins before laboratory results confirm the specific pathogen(s) involved. This approach is critical in preventing complications associated with untreated STIs, especially considering the asymptomatic nature of many infections. The selection of appropriate antibiotics hinges on understanding the pathogens involved and their susceptibility patterns.
In cases of Chlamydia trachomatis infections, the recommended first-line treatments include:
- Doxycycline: Administered as 100 mg orally twice daily for seven days, it is effective against a variety of bacterial STIs (Werner et al., 2025).
- Azithromycin: Administered as a single dose of 1,000 mg; it is particularly useful when compliance with a longer regimen may be challenging (Rodrigues et al., 2025).
The importance of selecting the right antibiotic cannot be overstated, as improper treatment can lead to persistent infections, exacerbating the risk of developing complications such as infertility or chronic pain syndromes (Rodrigues et al., 2025).
Recommended Antibiotics for Mixed Urogenital Flora
In treating mixed urogenital infections, several antibiotics have demonstrated effectiveness. The choice of antibiotic often depends on the specific pathogens identified and their susceptibility profiles. Here’s a comprehensive list of recommended antibiotics:
| Antibiotic | Dosage and Administration | Indications |
|---|---|---|
| Doxycycline | 100 mg orally twice daily for 7 days | First-line treatment for Chlamydia trachomatis |
| Azithromycin | 1,000 mg orally as a single dose | Alternative for Chlamydia trachomatis |
| Ceftriaxone | 1,000 mg IM or IV as a single dose | Empirical treatment for suspected gonococcal urethritis |
| Moxifloxacin | 400 mg orally daily for 7 days | For resistant Mycoplasma genitalium infections |
| Ciprofloxacin | 500 mg orally as a single dose | In cases where N. gonorrhoeae is confirmed sensitive |
The effectiveness of these antibiotics varies based on the pathogen involved and the local prevalence of antibiotic resistance. For example, in regions where resistance to azithromycin and doxycycline is common, alternative treatments such as moxifloxacin may be necessary.
Moreover, combination therapy may be utilized to cover the potential presence of multiple pathogens. For instance, in cases of suspected gonococcal urethritis, it is often recommended to combine ceftriaxone with doxycycline or azithromycin to ensure comprehensive coverage (Werner et al., 2025).
Prevention Strategies for Urogenital Infections
Preventing urogenital infections is critical for maintaining reproductive health and reducing the incidence of STIs. Here are several strategies that can significantly lower the risk of infections:
- Regular Screening: Routine screening for STIs, especially in high-risk populations, can facilitate early detection and treatment.
- Safe Sex Practices: The consistent use of condoms can reduce the transmission of STIs.
- Education and Awareness: Public health campaigns that educate individuals about the risks and prevention of STIs can empower them to take proactive measures.
- Timely Treatment: Prompt treatment of any diagnosed STIs can prevent complications and the spread of infections.
- Avoiding Douching: Women are advised against douching, which can disrupt the vaginal microbiome and increase susceptibility to infections.
By implementing these preventive strategies, individuals and healthcare providers can work together to mitigate the risk of mixed urogenital infections and promote overall reproductive health.
FAQ
What are the symptoms of urogenital infections?
Symptoms can vary depending on the specific infection but may include dysuria (painful urination), unusual discharge, itching, and pelvic pain.
How can I prevent urogenital infections?
Preventive measures include practicing safe sex, getting regular STI screenings, and maintaining good hygiene.
What is the best antibiotic for treating Chlamydia trachomatis?
Doxycycline and azithromycin are the most commonly recommended antibiotics for treating Chlamydia trachomatis infections.
Can urogenital infections lead to infertility?
Yes, untreated urogenital infections can lead to complications such as pelvic inflammatory disease, which significantly increases the risk of infertility.
Should I see a doctor if I think I have a urogenital infection?
Absolutely. Seeking medical advice is crucial for proper diagnosis and treatment to prevent complications.
References
-
Werner, R. N., Vader, I., Abunijela, S., et al. (2025). German evidence‐ and consensus‐based guideline on the management of penile urethritis. J Dtsch Dermatol Ges
-
Rodrigues, R., Sousa, C., Vale, N. (2025). Chlamydia trachomatis: From Urogenital Infections to the Pathway of Infertility. Genes. https://doi.org/10.3390/genes16020205
-
Abdel-Razek, M. A., Nazeih, S. I., Yousef, N. (2025). Analysis of a novel phage as a promising biological agent targeting multidrug resistant Klebsiella pneumoniae. AMB Express. https://doi.org/10.1186/s13568-025-01846-0
-
Gedefie, A., Getnet, S., Motbainor, H., Kassanew, B. (2024). Vaginal colonization and vertical transmission of Candida species: prevalence and associated factors among pregnant women and their neonates at public health facilities of Northeast Ethiopia. BMC Pregnancy Childbirth. https://doi.org/10.1186/s12884-024-07103-9