Table of Contents
What is Bacterial Vaginosis in Men?
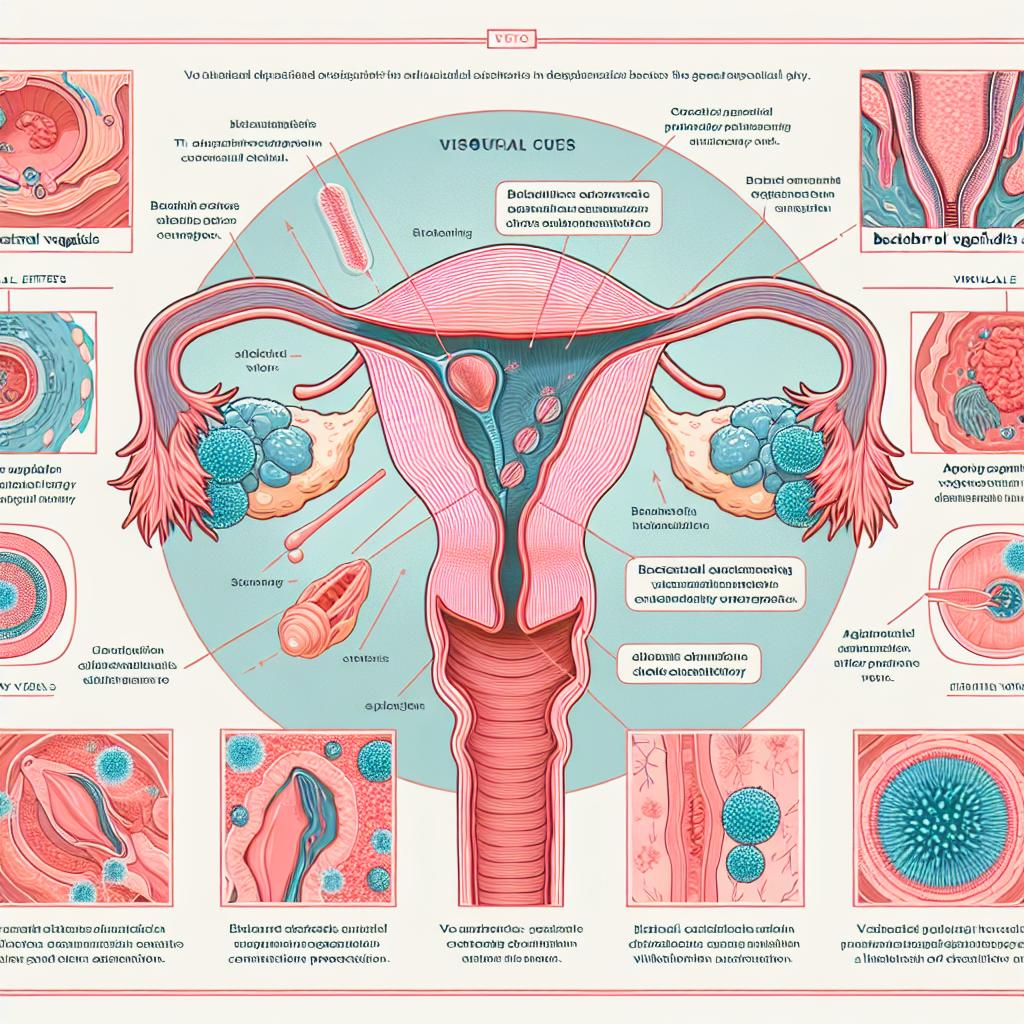
Bacterial vaginosis is a condition characterized by an imbalance in the normal bacterial flora of the vagina, leading to an overgrowth of certain types of bacteria. While BV predominantly affects women, men can also experience similar imbalances in their urogenital microbiome, particularly if they have sexual partners with BV. The condition can lead to various urogenital symptoms and can increase the risk of sexually transmitted infections (STIs).
Research indicates that the male microbiome is influenced by sexual activity and the presence of certain bacteria, such as Gardnerella vaginalis, which is often associated with BV in women (Orton & Monaco, 2024). The implication that men can harbor these bacteria suggests that BV in men may contribute to the transmission of infections and other health complications.
Symptoms of Bacterial Vaginosis in Men
The symptoms of bacterial vaginosis in men can vary and may not always be pronounced. Common symptoms may include:
- Unusual Discharge: Men may notice an unusual or foul-smelling discharge from the penis.
- Itching or Irritation: Some individuals may experience itching or irritation in the genital area.
- Pain During Urination: Dysuria or pain while urinating can occur.
- Discomfort During Intercourse: Men may feel discomfort or pain during sexual activity.
It is important to note that many men with bacterial vaginosis may be asymptomatic, meaning they do not exhibit noticeable symptoms but can still carry and transmit the bacteria to sexual partners (van Smoorenburg et al., 2025).
Causes and Risk Factors for Bacterial Vaginosis in Men
The exact causes of bacterial vaginosis in men are still being studied, but several factors may contribute to the condition:
- Sexual Activity: Having a sexual partner with BV increases the likelihood of a man developing the condition. The transmission of bacteria during intercourse can disrupt the natural balance of flora in the male urogenital tract.
- Multiple Sexual Partners: Men with multiple sexual partners are at a higher risk of contracting BV, as they may be exposed to various bacterial strains.
- Antibiotic Use: Recent use of antibiotics can disrupt the normal bacterial balance, leading to the overgrowth of harmful bacteria.
- Poor Hygiene Practices: Inadequate genital hygiene can contribute to bacterial imbalances.
Research indicates that the presence of Prevotella timonensis bacteria in the male urogenital tract can enhance susceptibility to HIV, further complicating the implications of BV in men (van Smoorenburg et al., 2025).
Diagnosis of Bacterial Vaginosis in Men
Diagnosing bacterial vaginosis in men can be challenging due to the nonspecific nature of symptoms. Healthcare providers may use several methods to diagnose the condition:
- Clinical Evaluation: A thorough medical history and physical examination are crucial. Doctors will inquire about symptoms, sexual history, and any partner’s BV diagnosis.
- Laboratory Tests: Urine tests or swabs may be performed to identify the presence of Gardnerella vaginalis or other BV-associated bacteria. Molecular diagnostic tests can also be utilized to assess the microbial composition of the genital tract (Neidhöfer et al., 2024).
- Symptom Assessment: Assessing symptoms and their severity can help clinicians determine the appropriate course of action.
It is essential for men experiencing symptoms or who suspect they may have BV to consult a healthcare provider for proper diagnosis and management.
Effective Treatments for Bacterial Vaginosis in Men
Treatment for bacterial vaginosis in men may vary based on the severity of symptoms and the presence of other infections. Common treatment options include:
- Antibiotics: Healthcare providers typically prescribe antibiotics such as metronidazole or clindamycin to treat bacterial vaginosis. These medications aim to restore the normal balance of bacteria within the urogenital tract.
- Partner Treatment: If a man is diagnosed with BV, it may be advisable for his sexual partner to undergo treatment as well to prevent reinfection and further transmission of bacteria.
- Probiotics: Some studies suggest that probiotics may help to restore a healthy microbial balance in the urogenital tract, although more research is needed in this area (Baimakhanova et al., 2025).
Table 1: Comparison of Treatment Options for Bacterial Vaginosis
| Treatment Option | Description | Effectiveness |
|---|---|---|
| Antibiotics | Metronidazole, clindamycin | High |
| Partner Treatment | Treating sexual partners | Prevents reinfection |
| Probiotics | Supplements to restore vaginal flora | Moderate (needs more research) |
It is important for individuals diagnosed with bacterial vaginosis to follow their healthcare provider’s recommendations and complete the full course of any prescribed medications.
FAQ
Can men get bacterial vaginosis?
Yes, men can experience bacterial vaginosis, although it is more commonly associated with women. Men may carry the bacteria without showing symptoms.
How is bacterial vaginosis diagnosed in men?
Diagnosis typically involves a clinical evaluation, laboratory tests, and an assessment of symptoms.
What are the treatment options for men with bacterial vaginosis?
Treatment options generally include antibiotics, partner treatment, and possibly probiotics to restore healthy bacteria levels.
Can bacterial vaginosis affect sexual health?
Yes, bacterial vaginosis can increase the risk of sexually transmitted infections, including HIV, and can affect sexual health overall.
How can I prevent bacterial vaginosis?
Practicing safe sex, maintaining good genital hygiene, and limiting the number of sexual partners may help reduce the risk of bacterial vaginosis.
References
-
Orton, K., & Monaco, C. (2024). The Vaginal Virome in Women’s Health and Disease. Microorganisms, 13(2), 431. https://doi.org/10.3390/microorganisms13020431
-
van Smoorenburg, M. Y., Remmerswaal, E. B. M., Segui-Perez, C., van Hamme, J. L., Strijbis, K., & Geijtenbeek, T. B. H. (2025). Vaginal Prevotella timonensis Bacteria Enhance HIV‐1 Uptake and Differentially Affect Transmission by Distinct Primary Dendritic Cell Subsets. Eur J Immunol
-
Neidhöfer, C., Condic, M., Hahn, N., Otten, L. A., Ralser, D. J., & Thiele, R. (2024). Homogeneity Between Cervical and Vaginal Microbiomes and the Diagnostic Limitations of 16S Sequencing for STI Pathogens at Higher Ct Values. Int J Mol Sci, 26(5), 1983. https://doi.org/10.3390/ijms26051983
-
Baimakhanova, B., Sadanov, A., Trenozhnikova, L., Balgimbaeva, A., & Orasymbet, S. (2025). Understanding the Burden and Management of Urinary Tract Infections in Women. Diseases, 13(2), 59. https://doi.org/10.3390/diseases13020059
-
van Teijlingen, N. H., Helgers, L. C., Zijlstra-Willems, E. M., & Geijtenbeek, T. B. H. (2024). Sexually Transmitted Infections and Bacterial Vaginosis in Women of Child-Bearing Age in Antananarivo, Madagascar: Prevalence and Risk Factors from a Cross-Sectional Study. BMC Infect Dis. https://doi.org/10.1186/s12879-025-10578-2
-
Bogaert, E., & Roels, R. (2025). Sexual health in patient care: shortcomings in medical training and experienced barriers in sexual history taking. BMC Med Educ, 25(1), 68. https://doi.org/10.1186/s12909-025-06850-3
-
Hlatshwayo, M., Reno, H. E., & Yarbrough, M. L. (2023). STI update: Testing, treatment, and emerging threats. Cleve Clin J Med, 90(3), 159-166