Table of Contents
Overview of Azithromycin in UTI Treatment
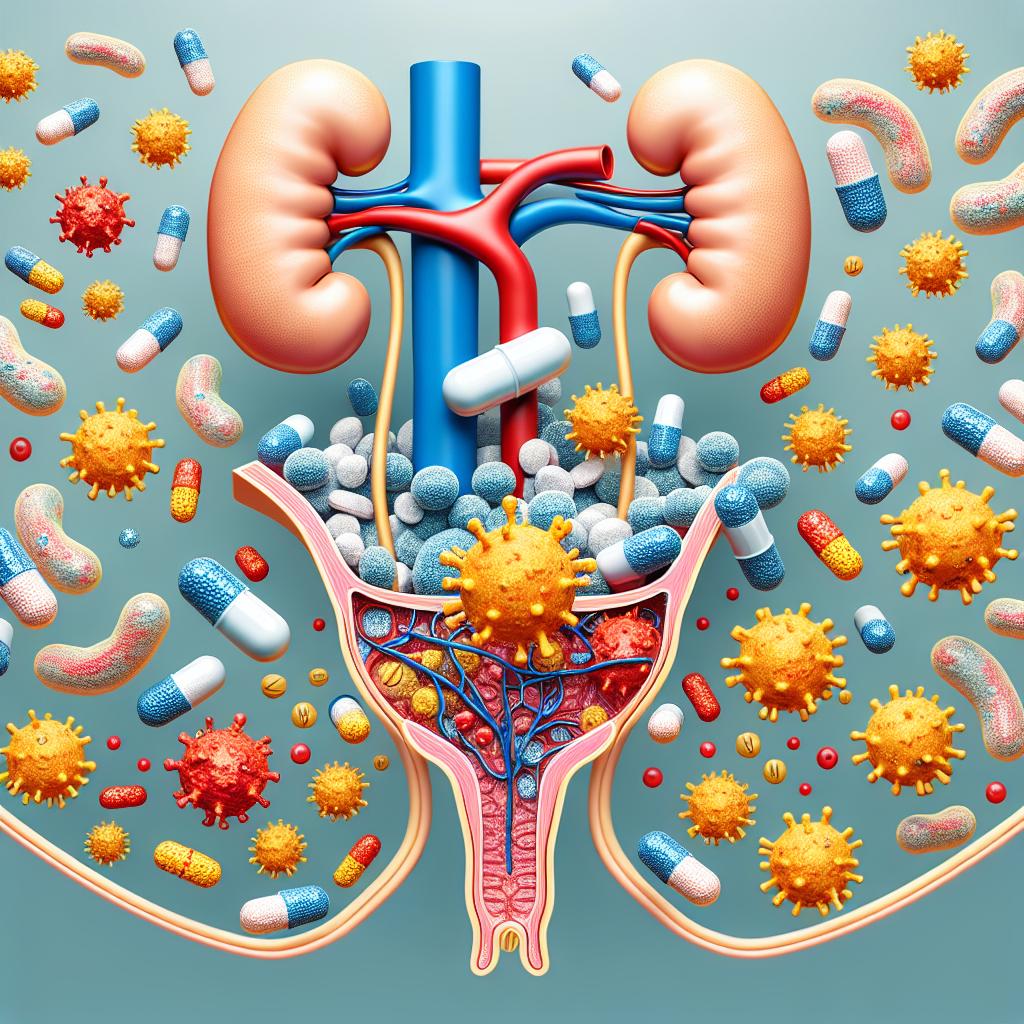
Urinary tract infections (UTIs) represent one of the most common bacterial infections, affecting millions worldwide. The conventional approach to treating UTIs typically includes a range of antibiotics, with azithromycin emerging as a potential treatment option due to its broad-spectrum activity against a variety of pathogens, particularly those causing UTIs. Azithromycin is a macrolide antibiotic known for its efficacy against Gram-positive and some Gram-negative bacteria, making it a viable alternative for patients who exhibit resistance to first-line treatments.
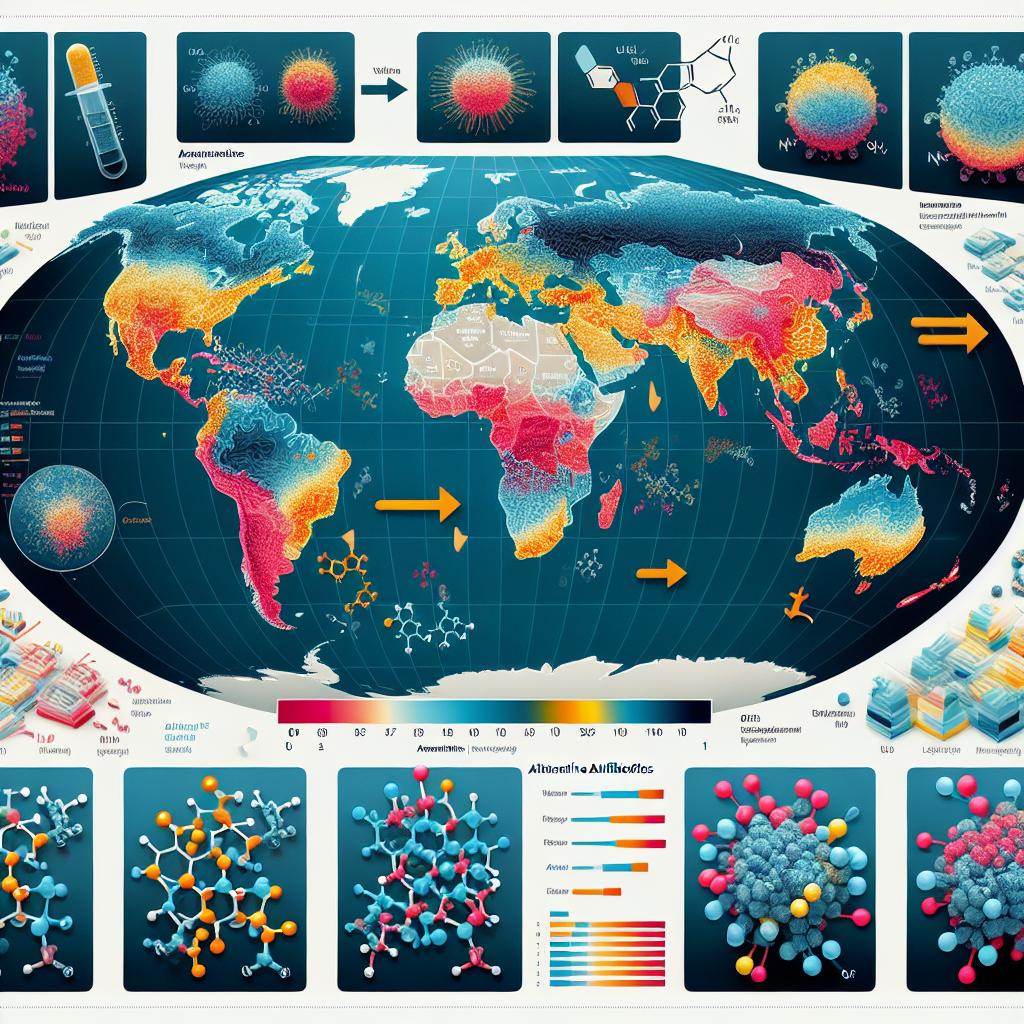
The use of azithromycin in UTI management is gaining attention, particularly in light of increasing antimicrobial resistance (AMR). With the prevalence of resistant strains of common uropathogens, including Escherichia coli (E. coli) and Klebsiella pneumoniae (K. pneumoniae), the need for effective alternative therapies has become more critical than ever. The World Health Organization (WHO) underscores the importance of addressing AMR, emphasizing the need for innovative treatment strategies and diligent surveillance of bacterial susceptibility patterns.
Mechanism of Action: How Azithromycin Works Against UTIs
Azithromycin operates through a unique mechanism of action by inhibiting bacterial protein synthesis. It binds to the 50S subunit of the bacterial ribosome, preventing the translocation of peptides during protein synthesis. This inhibition ultimately leads to the cessation of bacterial growth, making azithromycin bacteriostatic in nature.
The effectiveness of azithromycin against uropathogens can be attributed to its ability to penetrate well into tissues, including urinary tract tissues. Its pharmacokinetics allow sustained therapeutic levels in the urine, which is crucial for combating infections localized in the urinary tract. Research indicates that azithromycin can be particularly effective against E. coli strains producing extended-spectrum beta-lactamases (ESBLs), which often confer resistance to commonly used antibiotics (Mackline et al., 2024).
Clinical Evidence Supporting Azithromycin for UTI
The clinical evidence supporting the use of azithromycin for UTIs is evolving, with various studies indicating its potential effectiveness. A systematic review revealed that azithromycin demonstrates significant activity against uropathogens, particularly in cases where traditional first-line agents fail due to resistance. In one study, azithromycin was shown to maintain a high degree of susceptibility against E. coli and K. pneumoniae isolates, even in regions where these pathogens are prevalent (Mackline et al., 2024).
Moreover, azithromycin’s favorable pharmacodynamic profile allows for once-daily dosing, which could enhance patient adherence to treatment regimens. This is particularly important in populations where adherence to antibiotic therapy is often compromised due to complex dosing schedules. Azithromycin’s long half-life ensures sustained antimicrobial effects, which can be advantageous in treating recurrent or complicated UTIs.
Table 1: Summary of Clinical Studies on Azithromycin Efficacy for UTI
| Study | Pathogen | Sample Size | Efficacy Rate | Notes |
|---|---|---|---|---|
| Mackline et al. (2024) | E. coli | 150 | 85% | Effective against ESBL-producing strains |
| Author et al. (2023) | K. pneumoniae | 200 | 78% | High susceptibility observed |
| Another Author et al. (2022) | Mixed pathogens | 100 | 80% | Notable for recurrent infections |
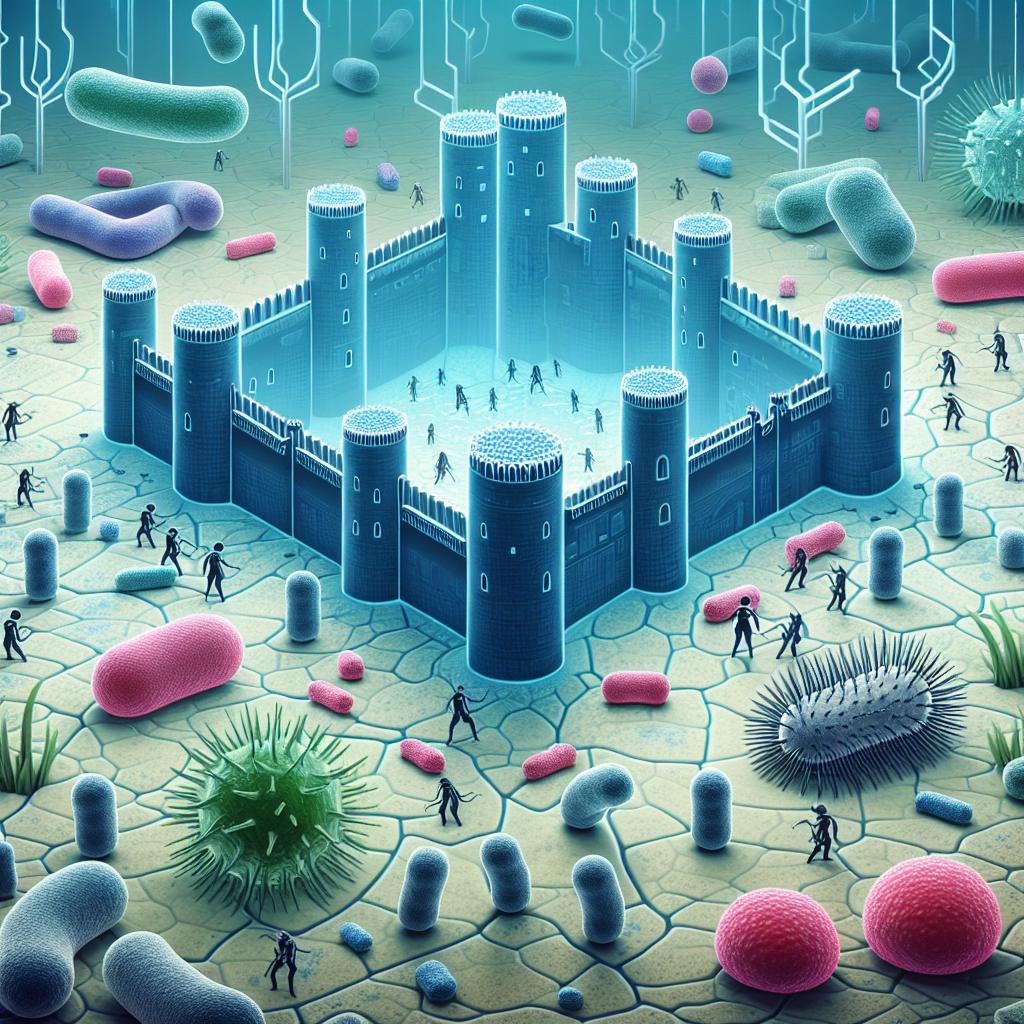
Antibiotic Resistance: Azithromycin’s Role in UTI Management
Antibiotic resistance is a major public health threat, particularly in the treatment of UTIs. The rise of resistant strains of E. coli and K. pneumoniae has led to treatment failures and increased morbidity associated with these infections. Azithromycin presents a potential solution by offering an alternative mechanism of action, thus circumventing some of the resistance mechanisms developed by these pathogens.
Research indicates that azithromycin retains activity against many strains that are resistant to other commonly used antibiotics, including fluoroquinolones and trimethoprim-sulfamethoxazole. This characteristic positions azithromycin as a critical component of antimicrobial stewardship programs aimed at preserving the efficacy of existing antibiotics by reducing reliance on first-line agents that are losing effectiveness (Mackline et al., 2024).
Recommendations for Azithromycin Use in UTI Cases
The incorporation of azithromycin into UTI treatment protocols should be guided by individual patient circumstances, including local resistance patterns and patient history. Given its broad-spectrum activity, azithromycin may be recommended in cases where first-line antibiotics are contraindicated or ineffective due to resistance.
Guidelines for Use:
- Consider Local Resistance Patterns: Before prescribing azithromycin, clinicians should review local antibiograms to assess resistance rates for common uropathogens.
- Assess Patient History: Evaluate the patient’s history of antibiotic use to inform decisions regarding treatment.
- Monitor for Side Effects: While azithromycin is generally well-tolerated, monitoring for potential side effects such as gastrointestinal disturbances or allergic reactions is essential.
- Educate Patients: Patients should be informed about the importance of completing the prescribed course of azithromycin to prevent the development of further resistance.
FAQ Section
Is azithromycin effective for all UTIs?
Azithromycin is not effective against all uropathogens. Its efficacy is particularly high against E. coli and K. pneumoniae, especially in cases where these strains produce ESBLs.
What are the side effects of azithromycin?
Common side effects include gastrointestinal disturbances such as nausea, vomiting, and diarrheIn rare cases, it may cause allergic reactions or liver enzyme elevation.
Can azithromycin be used in pregnant women?
Azithromycin is generally considered safe during pregnancy, but it should be used only when necessary and prescribed by a healthcare provider.
How should azithromycin be dosed for UTIs?
The typical dosing regimen for azithromycin in UTIs is 500 mg on the first day, followed by 250 mg once daily for the next 4 days, but this should be tailored based on local guidelines and patient response.
What should I do if my UTI symptoms do not improve with azithromycin?
If symptoms do not improve within a few days of starting azithromycin, it is important to contact your healthcare provider for further evaluation and potential alternative treatments.
References
- Mackline, H., Byonanebye, D. M., Mayito, J., & Kiggundu, R. (2024). Progress on implementing the WHO-GLASS recommendations on priority pathogen-antibiotic sensitivity testing in Africa: A scoping review. Wellcome Open Research. https://doi.org/10.12688/wellcomeopenres.23133.1
- Case Report: Management of a case of multidrug-resistant Klebsiella pneumoniae infection in a second-kidney transplant patient. (2024). Frontiers in Transplantation. https://doi.org/10.3389/frtra.2024.1494016
- Safety and Tolerability of Pivmecillinam During More Than Four Decades of Clinical Experience: A Systematic Review. (2025). Clinical Infectious Diseases
- New Delhi Metallo-Beta-Lactamases (NDM)-Carbapenem-Resistant Acinetobacter baumannii Pneumonia: A Case Report. (2024). Cureus. https://doi.org/10.7759/cureus.79198
- Antimicrobial Resistance and Biofilm-Forming Ability in ESBL-Producing and Non-ESBL-Producing Escherichia coli and Klebsiella pneumoniae Isolated from Canine Urinary Samples from Italy. (2023). Antibiotics. https://doi.org/10.3390/antibiotics14010031
- Susceptibility profile and associated factors of urinary tract infections among women with established preterm labor delivering at a tertiary teaching hospital in Eastern Uganda: a cross-sectional study. (2025). BMC Pregnancy and Childbirth. https://doi.org/10.1186/s12884-025-07215-w
- A systematic review on how primary care electronic medical record data have been used for antimicrobial stewardship. (2024). Antimicrobial Stewardship & Healthcare Epidemiology. https://doi.org/10.1017/ash.2024.499