Table of Contents
What Are UTIs and Their Common Symptoms?
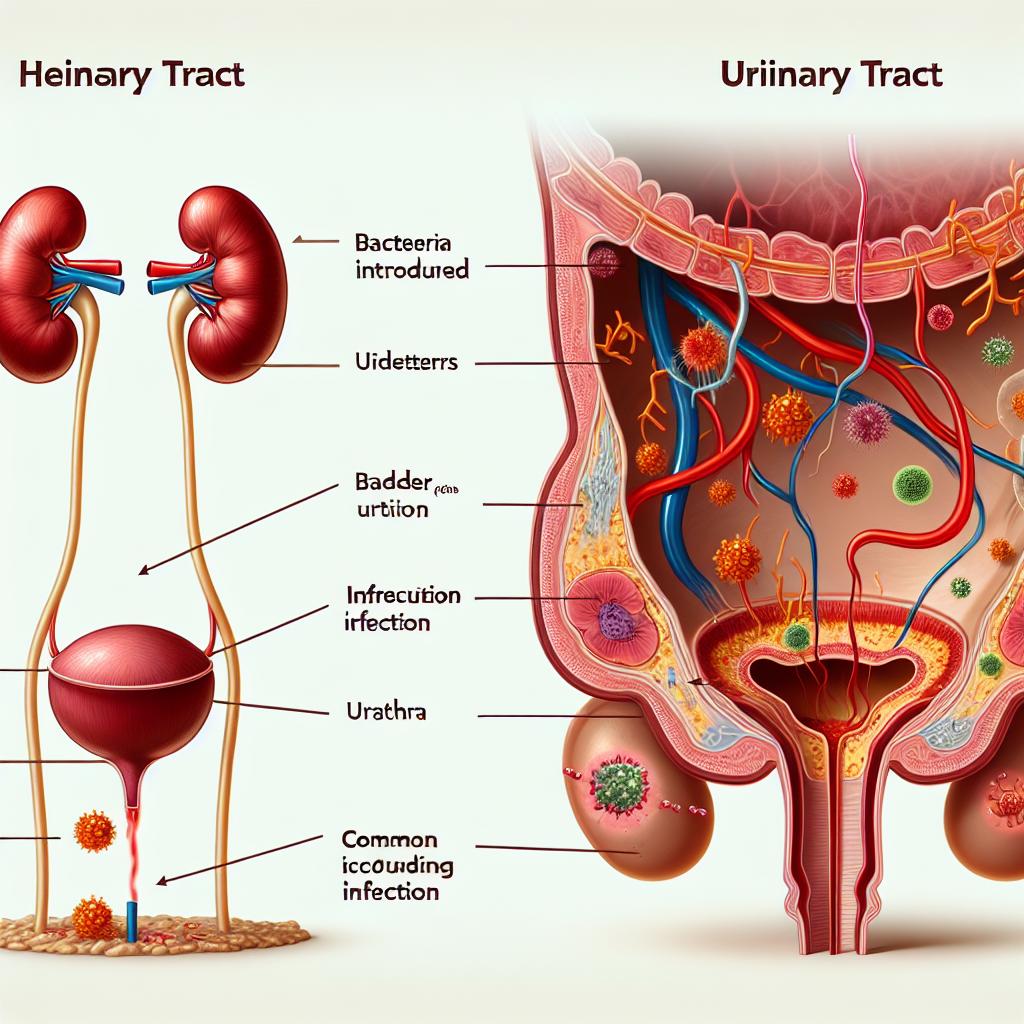
Urinary Tract Infections (UTIs) are infections that occur when harmful bacteria invade any part of the urinary system, which includes the kidneys, ureters, bladder, and urethra. UTIs are predominantly caused by bacteria, with Escherichia coli being the most common pathogen responsible for these infections.
Common symptoms of UTIs can vary in severity but typically include:
- Frequent Urination: An increased urge to urinate, often with little urine output.
- Burning Sensation: A painful or burning sensation during urination.
- Cloudy or Dark Urine: Urine may appear cloudy or dark, often with a strong odor.
- Pelvic Pain: Discomfort or pressure in the lower abdomen or pelvic area.
- Fever: Some individuals may experience fever or chills, indicating a more severe infection, especially if the kidneys are involved.
Recognizing these symptoms early is essential for prompt treatment, which can significantly reduce complications associated with UTIs (Mangwiro et al., 2024).
Understanding UTI Transmission: How Contagious Are They?
One of the most common misconceptions about UTIs is whether they are contagious. UTIs are not contagious in the traditional sense, as they do not spread from person to person like a cold or flu. However, certain behaviors and factors can increase the risk of developing a UTI, particularly in women.
Transmission can occur indirectly in the following ways:
- Sexual Activity: Sexual intercourse can introduce bacteria into the urinary tract, especially if proper hygiene is not maintained.
- Poor Hygiene: Inadequate personal hygiene can lead to bacterial growth and infection.
- Feminine Hygiene Products: Some products can irritate the urethra and lead to infections.
- Use of Catheters: Individuals who use catheters are at an increased risk as these devices can introduce bacteria directly into the urinary tract.
Overall, while UTIs themselves are not contagious, the conditions or actions that can lead to one may involve close contact with others (Ayele et al., 2024).
Factors That Influence UTI Contagion Risk
Several factors can influence the risk of developing a UTI, although they are not related to contagion:
- Anatomical Differences: Women are more prone to UTIs than men due to their shorter urethras, which allow bacteria easier access to the bladder.
- Hormonal Changes: Hormonal fluctuations, particularly during menstruation or menopause, can affect the urinary tract’s vulnerability to infections.
- Diabetes: High blood sugar levels can increase the risk of infections, including UTIs.
- Previous UTIs: Individuals who have had UTIs in the past are more likely to experience them again.
- Immune System Function: A weakened immune system can increase susceptibility to infections.
Understanding these risk factors can help individuals take proactive measures to reduce their risk of developing UTIs (Ayele et al., 2024).
Preventive Measures to Reduce UTI Spread
While UTIs are not contagious, there are effective strategies to prevent their occurrence. Here are some preventive measures:
- Hydration: Drinking plenty of fluids, particularly water, can help flush out bacteria from the urinary tract.
- Urinate After Intercourse: This can help remove any bacteria that may have entered the urethra during sexual activity.
- Wipe from Front to Back: This hygiene practice can prevent bacteria from the anal area from entering the urethra.
- Avoid Irritating Products: Steering clear of feminine hygiene sprays, douches, and powders can reduce irritation in the genital area.
- Wear Breathable Underwear: Cotton underwear allows for better air circulation, which can help prevent bacterial growth.
These preventive measures are vital for individuals at higher risk of UTIs, particularly women and those with a history of recurrent infections (Mangwiro et al., 2024).
Treatment Options for UTIs and Their Implications
UTIs are typically treated with antibiotics, which can effectively eliminate the infection. The choice of antibiotic may depend on the bacteria causing the infection and any previous antibiotic use. Common antibiotics include:
- Trimethoprim/Sulfamethoxazole
- Nitrofurantoin
- Fosfomycin
- Ciprofloxacin
It is essential to complete the full course of antibiotics as prescribed, even if symptoms improve before finishing the medication. Failure to do so can lead to antibiotic resistance, making future infections harder to treat.
In some cases, individuals may require follow-up testing to ensure the infection has cleared, particularly if they have recurrent Utis or if the infection was severe. Persistent symptoms or recurrent infections may require further evaluation to rule out underlying conditions, such as kidney stones or anatomical abnormalities (Gadisa et al., 2024).
Table 1: Common UTI Treatments and Their Typical Uses
| Antibiotic | Typical Use |
|---|---|
| Trimethoprim/Sulfamethoxazole | First-line treatment for uncomplicated UTIs |
| Nitrofurantoin | Effective for lower urinary tract infections |
| Fosfomycin | Used for uncomplicated UTIs, especially in pregnant women |
| Ciprofloxacin | Generally reserved for complicated UTIs or resistant strains |
FAQ
Can you get a UTI from someone else?
No, UTIs are not contagious. They occur when bacteria enter the urinary tract, often related to personal hygiene or sexual activity.
How can I prevent UTIs?
Stay hydrated, urinate after intercourse, practice good hygiene, and avoid irritants in the genital are
What are the symptoms of a UTI?
Common symptoms include frequent urination, burning during urination, cloudy urine, and pelvic pain.
How are UTIs treated?
UTIs are typically treated with antibiotics prescribed by a healthcare provider. It is crucial to complete the entire course of medication.
Are there any long-term effects of UTIs?
If left untreated, UTIs can lead to more serious infections, such as kidney infections. Recurrent UTIs may require further investigation.
References
-
Ayele, B., et al. (2024). Whole genome sequencing and antimicrobial resistance among clinical isolates of Shigella sonnei in Addis Ababa, Ethiopia. PLoS One. Retrieved from https://doi.org/10.1371/journal.pone.0313310
-
Gadisa, E., et al. (2024). Epidemiology, antimicrobial resistance profile and management of carbapenem-resistant Klebsiella pneumoniae among mothers with suspected sepsis in Ethiopia. Ann Clin Microbiol Antimicrob. Retrieved from https://doi.org/10.1186/s12941-024-00745-9
-
Mangwiro, L., et al. (2024). Determinants of neonatal mortality among hospitalized neonates with sepsis at Queen Elizabeth Central Hospital, Blantyre, Malawi: A mixed-methods study. PLOS Global Public Health. Retrieved from https://doi.org/10.1371/journal.pgph.0004059